Other Eye Treatments
There are a large number of conditions that can affect the eye. Sadly, due to aging factors the number of eye problems we experience can increase. Kent Eye Centre are happy to provide a thorough investigation to help determine the route cause of any concerns you may have about your eyes.
There are specific sub categories in which Kent Eye Centre specialise in, follow the links below to find out more.
Glaucoma
Glaucoma is the name given to a group of eye conditions that causes optic nerve damage and can affect vision.
Dry Eye
Dry eye occurs when people don't have enough tears on the surface of their eyes to lubricate the eyes and keep them comfortable.
Keratoconus
Keratoconus is a condition in which the shape of the cornea, which is usually round, is distorted, developing a cone-shaped bulge, resulting in harm to vision.
Retina
The Retina is a thin film of nerve tissue that fans out from the optic nerve and lines the back of the eye.
Glaucoma
What is glaucoma?
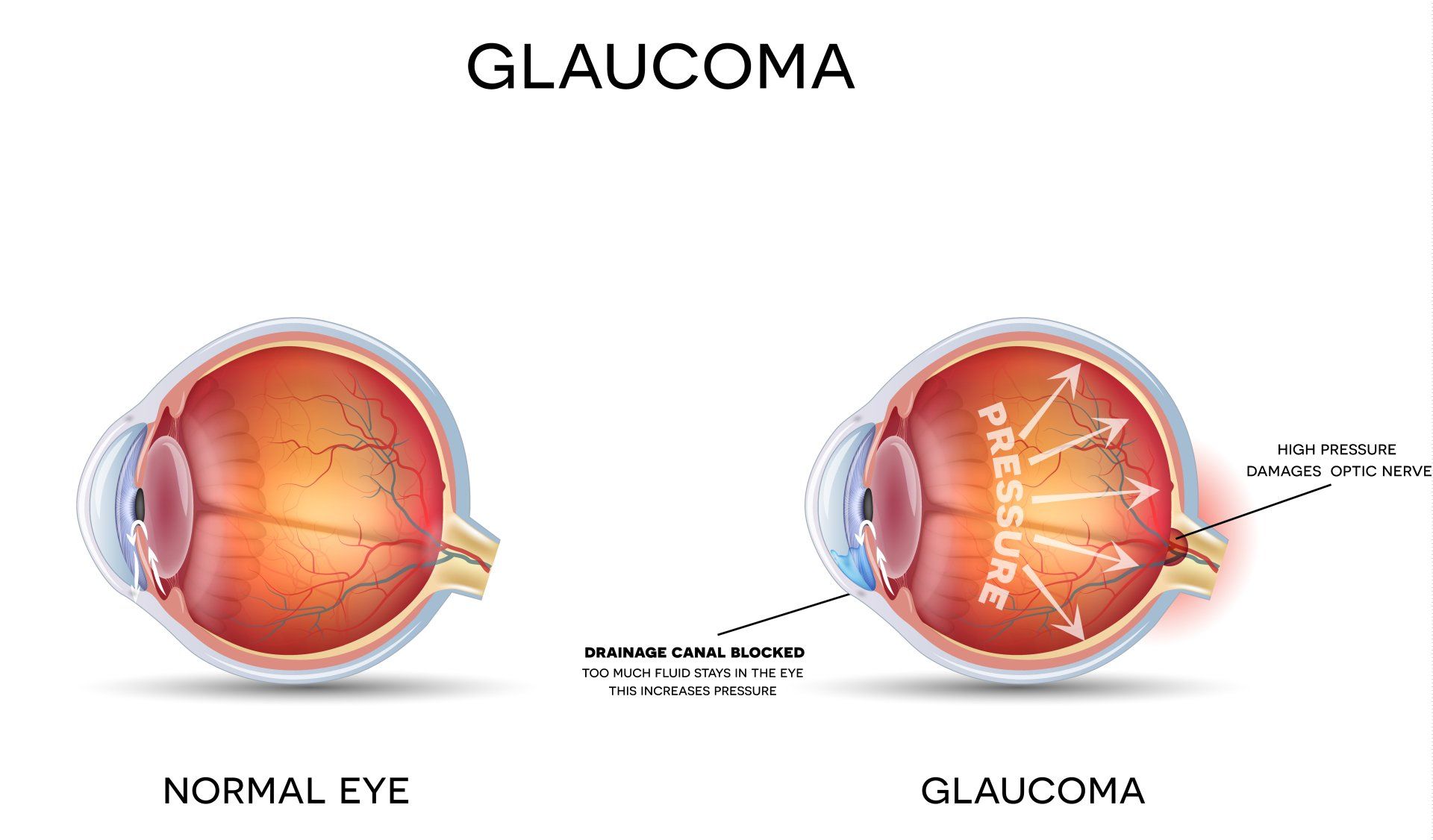
Glaucoma is an eye condition where your optic nerve is damaged by the pressure of the fluid inside your eye.
This may be because your eye pressure is higher than normal, or because of a weakness to your optic nerve. Your eye needs a certain amount of pressure to keep the eyeball healthy and in the right shape. But if the pressure is too high, it can cause your optic nerve to become damaged at the point where it leaves your eye. This damage is called glaucoma.
What are the types of glaucoma?
The main types of glaucoma are:
- Primary open angle glaucoma: the most common type of glaucoma in the UK. It’s also known as chronic open angle glaucoma which means the damage to your optic nerve and changes to your sight happen very slowly over time.
- Closed angle glaucoma: where damage to the optic nerve can happen very quickly due to a sudden rise in eye pressure.
- Normal tension glaucoma: when an eye pressure within the normal range still causes damage to the optic nerve.
- Secondary glaucoma: which occurs as a result of another eye condition, an injury to the eye or due to medication.
How can glaucoma affect my sight?
Most types of glaucoma have no symptoms, so a regular eye test at your opticians is the only way to know you have the condition. You may not notice any difference in your vision because glaucoma affects your peripheral vision (also known as your side vision) first. As your peripheral vision is not as sensitive as your central vision, it’s difficult to notice any early changes to your vision – but your sight is being damaged.
Because you may not notice a problem until your glaucoma is more advanced, it’s important to have regular eye tests as this is the only way to know if you have it. The earlier your glaucoma is picked up and treated, the more of your sight can be protected.
What is the treatment for glaucoma?
All treatment for glaucoma aims to lower your eye pressure to prevent damage to your optic nerve and your sight.
Treatment to lower your eye pressure usually starts with eye drops, and for most people with glaucoma, this is all the treatment they will ever need. But, these drops will need to be used long term or for life.
If it’s not possible to control your eye pressure with eye drops alone, your ophthalmologist may suggest other treatment.
In a very small number of people with glaucoma, where eye drops haven’t been successful in keeping the eye pressure stable, or where the glaucoma is advanced, surgery may be an option. Here at Kent Eye Centre we offer the latest innovative surgery called i-Stent click here to find out more.
Managing your glaucoma
Most people with glaucoma use eye drops for many years or for life. Using your drops regularly helps to keep your eye pressure under control and prevents damage to your sight. Not using your drops could, in the long term, make your glaucoma unstable and lead to permanent sight loss. Unfortunately, once sight loss due to glaucoma has occurred, it is not reversible.
It’s also very important to attend all your appointments at the eye clinic to make sure your eye pressure stays stable. This is because changes in eye pressure have no symptoms, and without regular checks you won’t be able to tell that your treatment is working. How often you need to be seen at the eye clinic will depend on how well your treatment is working.
Ocular hypertension (high eye pressure)
Some people naturally have eye pressure above the normal range, but this pressure doesn’t cause any damage to their optic nerve. This is described as ocular hypertension rather than glaucoma. Some people’s optic nerves stay healthy at higher than normal eye pressures.
If you have ocular hypertension, it can increase your risk of developing glaucoma so this needs to be monitored. Sometimes you may be prescribed eye drops to help reduce your eye pressure and reduce your risk of developing glaucoma. If this is the case, you’ll be followed up at the eye clinic regularly to monitor your eye pressure. You may be discharged from the eye clinic if you don’t require eye drops and tests show that there is no sign of glaucoma. However, it’s important for you to visit your optometrist (optician) regularly for your eyes to be checked so that any future changes can be picked up.
Dry Eye
What is dry eye?
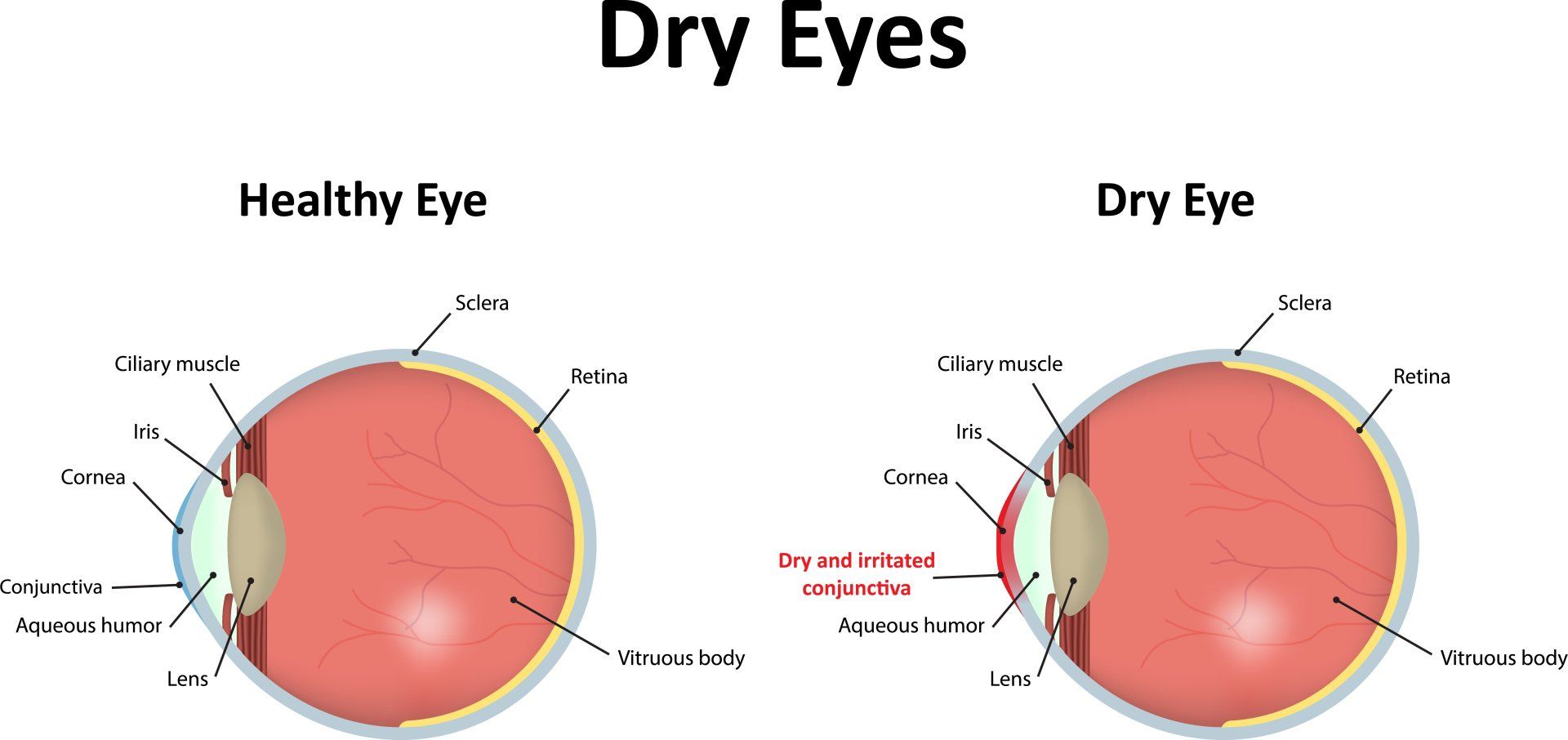
Dry eye is an eye condition caused by a problem with your tears.
Dry eye can make your eye feel uncomfortable, red, scratchy and irritated. Despite the name, having dry eye can also make your eyes watery. Typically, dry eye doesn’t cause a permanent change in your vision. It can make your eyesight blurry for short periods of time, but the blurriness will go away on its own or improve when you blink.
Why have I developed dry eye?
Dry eye is caused by a problem with your tears. You can develop dry eye if you don’t produce enough tears, or the tears aren’t of the right quality or if they don’t spread across the front of your eye properly.
Dry eye is usually more common as people get older. As we age, our eyelids aren’t as good at spreading tears each time we blink. The various glands in our eyes that produce tears may also become less effective. It is not always known what causes your eye to become dry but essentially, the quality of something known as your tear film gets worse.
What is the tear film?
When you blink, you spread a thin layer of liquid, called the tear film, over the front surface of your eye. The tear film keeps the front surface of your eye healthy and it also helps the eye focus properly, giving you clear vision.
The tear film is made up of three layers: the mucin (mucous) layer, the aqueous (watery) layer, and the lipid (oily) layer. Each one of these layers is needed to keep your tear film healthy.
Anything that affects the structure and balance of your tear film – for example if you produce too little or too much of one of the layers – will stop the tear film working properly and potentially cause dry eye.
What are the causes of dry eye?
It is sometimes difficult to determine the exact cause of dry eye. Dry eye is multifactorial, which means that that there can be many factors that contribute to the condition. Sometimes dry eye can be connected to other conditions affecting your body such as diabetes or rheumatoid arthritis. The condition is common in both men and women.
Medication
If you’re taking certain drugs, such as antihistamines, antidepressants, pain medications and oral contraceptives, you may develop dry eye symptoms. Eye drops which contain preservatives may also contribute to dry eye, especially if you are using them frequently.
Contact lenses
Using contact lenses can cause you to develop dry eye. The length of time you wear your contact lenses along with other factors such as using computer screens, air pollution and wearing make-up can make the symptoms of dry eye worse. You should follow the advice for wearing contact lenses issued by your optometrist in terms of replacement frequency, wearing time and cleaning regime.
Other health conditions
There are a number of health conditions, particularly inflammatory conditions, that are associated with dry eye, such as rheumatoid arthritis and Sjögren’s syndrome. Sjögren’s syndrome is a condition that may cause you to have dry eye and a dry mouth.
Surgery to the eye or injury to the eye surface
If you have surgery on your eye (for example laser eye surgery) or an accident which affects or scars your eye, you may develop dry eye. Your dry eye symptoms usually improve once the eye has healed, but this can take time.
Environment
There are environmental factors that may cause or make your dry eye symptoms worse. These include dusty or smoky environments as well as heavily polluted areas or wearing make-up. Using air conditioners in the car and office as well as heaters may make your dry eye symptoms worse. Trying to identify and address these environmental factors are often recommended as a first step in helping to reduce your dry eye symptoms. Using air purifiers and humidifiers might help.
What is the treatment for dry eye?
There’s no cure for dry eye but there are treatments that can help your eyes feel more comfortable and keep your symptoms at bay.
If your dry eye is caused by medication, then your GP may consider switching your medication to another. If your dry eye is caused by wearing contact lenses, then having a break from your lenses or asking your optometrist about trying a different type of contact lens may help the dry eye to improve.
Often dry eye is caused by getting older, which can’t be helped, but there is treatment that can help with your symptoms. There are three main ways to help your dry eye:
- making the most of your natural tears
- using artificial tears (eye drops)
- reducing the draining away of the tears.
Making the most of your natural tears
There are things that you can do yourself which may help reduce the symptoms of dry eye. High temperatures and central heating can make tears evaporate more quickly, so sometimes lowering temperatures can help. Many people find that their dry eye is worse when they’re reading or using a computer. This is because you blink less when you are doing a task like this, giving the tears more chance to evaporate. You can try to blink more when you’re doing these tasks, or use eye drops before you read, watch TV or use a computer, as this may help to keep your eyes comfortable.
Using eye drops
Most people with dry eye need to use some form of eye drops, also known as artificial tears. Eye drops aim to supplement and replace your natural tears and help keep the surface of the eyes lubricated. This can make the eyes feel more comfortable. They can also prevent any damage to the front of your eye, which can happen if the eye is dry for a long time.
You should use your eye drops as advised. If you are having to use your drops more than four times a day, then you should let your ophthalmologist or optometrist know, as you may need a different type of drop or additional treatment to the drops you’re using.
Reducing the draining away of tears
It’s possible to help dry eye by blocking up the drainage holes, called puncta, in your eyelids. Stopping the tears from draining away may help your tears stay in your eye for longer. The medical term for blocking the tear ducts is “punctal occlusion”.
Usually, punctal occlusion is tried for a period of time to see if it helps. The small drainage channels are blocked by small devices called punctal plugs. If it helps you with the symptoms of dry eye then the plugs are left in place. Occasionally, a permanent small surgical procedure can also be performed, if temporary blocking has been useful.
Often plugs or blocking the ducts is helpful at reducing the number of drops you need to use in the eyes every day. If you’ve had your tear ducts blocked you may still need to use drops, gels or ointments to protect your eyes and keep them as comfortable as possible. Here at Kent Eye Centre we offer a full diagnostic consultation with management plans and the option for punctal occlusion if necessary.
Keratoconus
What is Keratoconus?
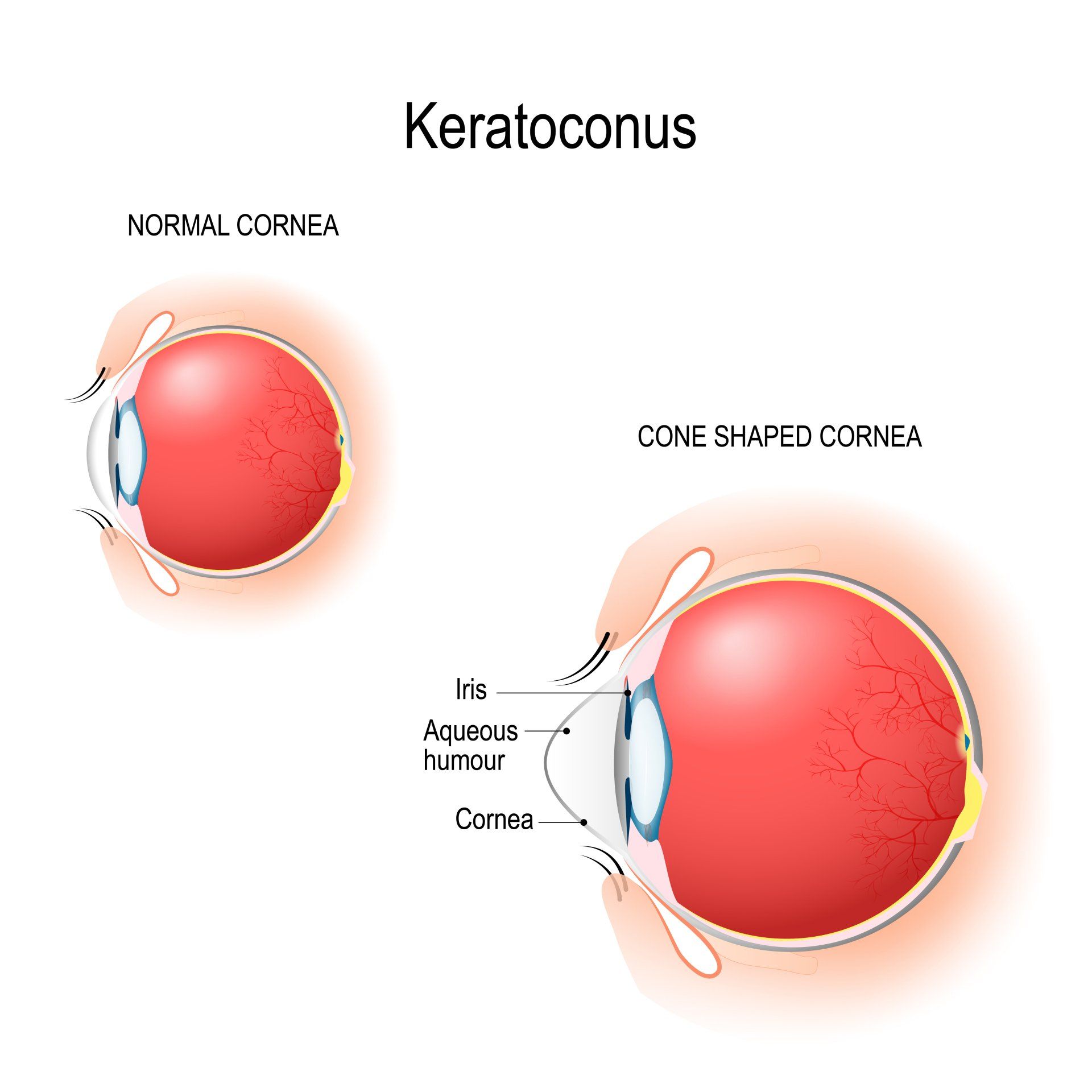
Keratoconus (keh-rah-toe-cone-us) affects your cornea, the clear dome-shaped window at the front of your eye. Your cornea focuses light into your eye to help produce a clear image. In keratoconus, your cornea becomes weaker and thinner at its centre. This thinning causes it to bulge outwards in an irregular cone shape. This can make your vision blurry and distorted, as light being focused by your cornea forms an unclear image on your retina, at the back of your eye.
Keratoconus usually develops in your teens or 20s and can worsen over time. It cannot be treated with eye drops or other medications. In the early stages, glasses may help correct vision. As keratoconus develops glasses may no longer help, but most people can still get a good level of vision by wearing contact lenses. Depending on your keratoconus sometimes contact lens can be uncomfortable to wear for long periods.
Are there any treatments that can help to slow down keratoconus?
Collagen cross-linking, also known as CXL or C3R, is a treatment used to treat progressive (worsening) keratoconus. The aim of this treatment is to stop things getting worse, although, for some people cross-linking can also cause an improvement.
The middle layer of your cornea, the stroma, is made up of a web of collagen fibres held together with links. This gives your cornea its shape and strength. In keratoconus these links may be less strong causing your cornea to bulge outwards in an irregular cone shape.
It is thought that CXL works by increasing the number of naturally occurring collagen cross-links in your cornea, making it stronger. Treatment can be carried out by an ophthalmologist or sometimes nurse specialist and involves removing a small area of the surface of your cornea, known as the epithelium, and then applying vitamin B2 (riboflavin) drops. Your cornea is then exposed to ultraviolet-A (UVA) light.
The main aim of CXL is to stop keratoconus getting worse, preventing your vision from deteriorating in the future. For some people this treatment can also help to flatten and regulate the shape of your cornea, improving vision, although this is not the case for everyone. Cross-linking is usually carried out on one eye at a time, and may need to be repeated.
There is some promising evidence that CXL is very successful in stopping the development of keratoconus and more evidence is being collected all the time, to help CXL become a regular treatment.
Other treatments
Corneal implants are flexible C-shaped plastic rings which are inserted into the edges of your cornea. These aim to flatten the cornea, to correct its irregular shape. For some people this can allow for a better contact lens fit or better correctable vision with glasses.
Usually two C-shaped rings are inserted and this procedure can be done under local or general anaesthetic (while you are awake or asleep). A small cut is made in the cornea and channels are created into which the implants are placed.
At the moment there is no good evidence that shows that corneal implants prevent worsening of, or reverse keratoconus.
Are these treatments available on the NHS?
Corneal implants and epithelium‑off collagen cross-linking aren’t routinely available on the NHS.
Although the National Institute for Health and Care Excellence (NICE), the body that approves treatments for use on the NHS, has said that corneal implants and epithelium‑off cross-linking work well enough and are safe enough to use on the NHS, at present the is no guidance that these treatments should receive routine NHS funding. This means that these treatments are not available everywhere.
Some hospitals offer CXL as routine but others may not. If your ophthalmologist feels that these treatments would be suitable for you, they may need to apply for specific funding from your local health provider for you to receive them.
Here at Kent Eye Centre we offer a full diagnostic consultation with management plans and the option for surgical treatment if necessary.